13 On Your Side Exclusive: Missing a Memory
Navigating through Alzheimer's
YUMA, Ariz. (KECY/KYMA) - You may all know the feeling of forgetting your keys or phone at home. But what if you began to forget the name of your loved one...or perhaps precious memories?
I spoke to the daughters of a Yuma resident who knows about the fear of forgetting.
Sisters Lorri Nienaber and Lynene Voelker know the fear of forgetting all too well.
“It’s always why my mom? Why did this happen to a woman who’s been perfectly healthy her whole life, and she had this great life, and then to be diagnosed with something like this?” said Nienaber.
“It’s changed the way that we live a lot,” said Voelker. “It changed our life because Greg [my husband] and I lived in California and when we got the diagnosis, we were in a situation where we could pack up and move, and we literally in three months packed up our stuff and moved to Yuma and we’ve been here a year and a half because of my mom. We want to be able to spend as much time with her as we can while she is still in the stage that she’s in, and while she remembers us,” said Nienaber.
“We spend a lot more time together as a family. With my parents, we spend almost every Friday night with them. A group of us go out every Thursday night, we have dinner at Lorrie’s house, we try to keep my mom involved, and get my dad out because he is her caretaker,” said Voelker.
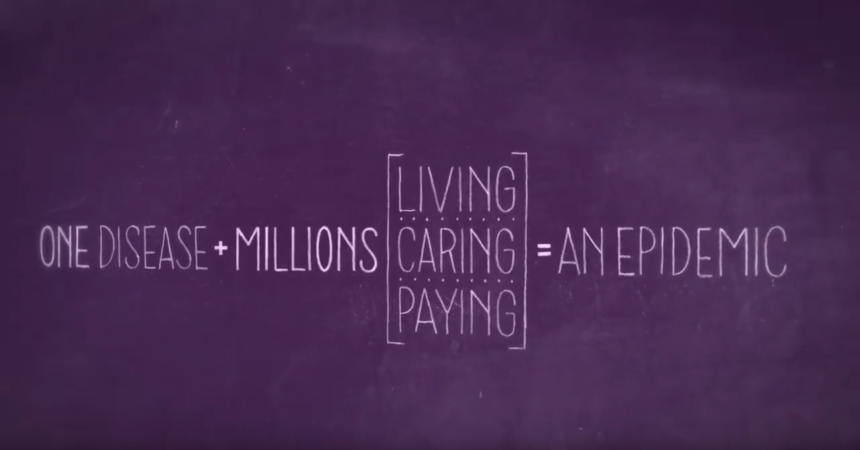
There are currently an estimated 50 million people living with dementia, and Lecil Nienaber is one of them.
“We are blessed that she has finally accepted this and is a good spirit about it because otherwise, I think it would be really difficult,” said Nienaber.
Some people with Alzheimer’s also react differently to the symptoms of the disease.
“It’s more just daily tasks of remembering little things. Like maybe where she put something in the kitchen, or you will ask her ‘what did you and dad do today?’ and she will say ‘nothing,’ or ‘I don’t remember.’ But they had been out and been to the grocery store, or she went to the doctor or something,” said Nienaber.
“We came up with a plan that I did. I called my dad and said ‘how about if we tell her her grandkids are worried about her.’ So I made those phone calls to my mom and I just said ‘Mom, Bryce and Courtney, and Amber notice that when they talk to you, you are not remembering things,’ and she says ‘oh, I don’t?’ And I said ‘well, they are a little concerned that you repeat yourself, and I think it would make your grandchildren really happy if you went to the doctor, and talk to the doctor about your memory.’ And she said ‘OK.’ That’s all it took. So then she went to the doctor, and she said ‘why am I here again?’ I said ‘remember your grandkids are worried about you, you need to have your memory tested.’ And she said ‘OK,’” said Nienaber.
“She’s very aware that she doesn’t remember. She will tell you ‘I don’t remember.’ There is no denial,” said Voelker.
If you learn what to expect from the disease, you can help your loved one with their fear of the unknown.
“What’s going to happen when mom wakes up one morning and looks at my dad and says ‘who are you?” said Nienaber.
It is important to keep lines of communication open as the symptoms of the disease get worse.
“I think people put that conversation off for a long time because they think they might hurt their loved one's feelings, and it might upset them by talking about it. But what we find is that the earlier families have these conversations, and these kinds of compassionate and caring conversations happen, the earlier that diagnosis is going to happen,” said Morgen Hartford, the regional director of the Alzheimer’s Association, desert southwest chapter.
For someone living with Alzheimer's or dementia, remember that they are still the same person.
“She has dementia, she’s perfectly fine, and they say ‘oh Liesel, how are you today?’ and they talk to her like a child,” said Nienaber. ”Just treat her like you did before you found out she has dementia. You see a change in people and how they treat someone with dementia,” she continued.
In 2019 Alzheimer’s affected 16 million caretakers nationwide like Lorri and Lynene, who provide unpaid care for people living with the disease.
“In Arizona, there are 339,000 caregivers today and they are providing unpaid care to their loved ones. They are not getting paid for the care that they provide and that is certainly an economic drain on the state and an economic drain on the family,” said Hartford.
“My dad is an awesome caretaker, he stepped right in and took over the bill pay, and took over everything,” said Voelker.
“It will, of course, become a burden financially. My mom and dad have always managed their money well, and I know that my dad worries about it. He’s been financially planning out what’s going to happen if that day does come,” said Nienaber. “I cannot even imagine my dad not having us to help with this,” she continued.
During 2018 the cost of unpaid care for those with Alzheimer's was estimated to total over 4 billion dollars in Arizona.
Because of the staggering numbers and financial hardship of the disease, it is normal for both the caretaker and the individual to go through a range of emotions after receiving a diagnosis.
“I don’t think it was hard to accept because the progression was so slow,” said Voelker.
“The diagnosis was a little shocking. To actually hear those words come out of the neurologist’s mouth…I think I cried for about three hours,” said Nienaber.
If you are a caretaker, know that your emotions are also important.
Neglecting your own well-being can be harmful to you and your loved one.
“Everybody is always worried about the person who has dementia, which I get, but nobody thinks about the kids, the caregiver, my dad. We make sure that our dad takes care of himself first because what’s that’s what’s most important. If he can’t take care of himself, he certainly can’t take care of her,” said Nienaber. “His health is very important, and they say that the caregiver gets forgotten about. Nobody thinks about the caregiver, and I’m sure there’s going to come a time where we might be the primary caregiver of the both of them,” she continued.
As the disease progresses, you will need the support of those who know and understand you, for the caretaker and a person diagnosed with Alzheimer’s.
“They often feel isolated, and I think the most important thing for the caregivers to know, is that they’re not alone,” said Hartford.
“Once you open up to people, you find out how many people’s parents and grandparents have it, but nobody wants to talk about it,” said Nienaber.
Since 2000, there has been a 193% increase in Alzheimer’s deaths in the state of Arizona.
In San Diego and Imperial counties, more than 60,000 people are living with Alzheimer’s disease and more than 160 thousand family and friends are providing care.
“Arizona has the fastest growth rate of Alzheimer’s disease in the entire US,” said Hartford.
While the terms “Alzheimer’s” and “dementia” are often used interchangeably, there are distinct differences between the two.
“If you think about dementia as a general umbrella, dementia is a collection of symptoms that include changes in memory, change in behavior, and judgment, reasoning, changes in vision, and balance. Alzheimer’s is a specific disease that has to do with the hallmark changes in someone’s brain. Having a buildup of plaques and tangles, proteins in the brain that go on to lend themselves to the symptoms with Alzheimer’s disease,” said Hartford. “The primary risk factor for Alzheimer’s is age, and with Arizona being a retirement state, a lot of people come here for the beautiful weather. We have more older people over age 65,” he continued.
Today, we know that Alzheimer’s is a brain disease that impacts memory, thinking, and behavior.
“Her long-term memory is excellent, her short-term memory is not so great, it’s pretty much shot,” said Nienaber.
“You think of Alzheimer’s primarily as an association to memory, but also know that there are many forms of dementia, not just Alzheimer’s. Alzheimer’s is the most common form, but it doesn’t always include memory. Some things can include changes in vision, balance, word-finding, misplacing things that you don’t usually misplace. Those subtle things sometimes can be shrugged off as normal aging. What people need to know, is that if it’s outside the norm for you, if you’ve always been good at remembering names, it’s something to be concerned about,” said Hartford.
Alzheimer’s disease causes nerve cells to die, which leads to brain tissue loss or shrinkage, and causes loss of function and communication between the cells.
“What we also tell people is, don’t assume it’s Alzheimer’s disease. Many different conditions can cause some of the changes and symptoms we talk about with dementia, but it’s not necessarily Alzheimer’s. Things like thyroid conditions, or vitamin deficiencies, all those things can make a difference in how people learn and reason,” said Hartford.
To this day scientists are still unsure of why this happens but they have identified certain risk factors that increase the chances of developing Alzheimer’s such as age, family history, and genetics.
“If you have what is known as the APOE4 gene, that’s the age-related gene for Alzheimer’s disease. So you’re going to be at a higher risk if you have one or more family members with the disease. You’re going to be at an increased risk, know that’s not a determinator, that’s not saying you will get Alzheimer’s disease, but it tells you your risk may be higher,” said Hartford.
In the state of Arizona, in the year 2019, there were 140,000 people age 65 and up with Alzheimer’s and it is estimated that number will increase by 42 percent by the year 2025.
“One in nine people age 65 and up have Alzheimer’s disease. That goes up to one in three at age 85,” said Hartford.
As of 2020, there is still no cure for Alzheimer’s and no proven way to stop the death of brain cells.
There are, however, non-drug treatments and medications that may help with symptoms.
“We do have some promising medications that are on the horizon, both to reduce the symptoms of the disease, and the actual effects of the disease in the brain,” said Hartford.
Alzheimer’s often progresses slowly in three typical stages: early, middle, and late.
“When she does remember she has it, she thinks about it all the time. It’s always in her mind,” said Nienaber.
The symptoms of the disease worsen over time but the rate of progression varies from person to person.
On average, a person with Alzheimer’s may live four to eight years after they have been diagnosed but can live as long as twenty years depending on the diagnosis.
“Her neurologist told us she could be this way for the next 10 years or the next 20 years. You can’t predict the progression,” said Voelker.
“She does testing every six months, she does a memory test. The last time she was 26% worse six months earlier,” said Nienaber.
“We want people to be diagnosed as early as possible because when you find that effective intervention, the goal is to stop the disease in its tracks. If there are things we can do to reverse the effects of the disease of dementia, we want people to find that, and make that diagnosis as early as possible,” said Hartford.
“She was in denial at first. She didn’t want anybody to know, but now we don’t think she knows she has dementia. She just knows that there’s something wrong with her brain. She’ll say ‘oh I think I’m going to the brain doctor,’ but she doesn’t know why she’s going. And she knows she doesn’t remember things, but if you tell her ‘mom remember that you have dementia,’ she will say ‘oh I do?’” said Voelker.
“The downhill starts is when they stop remembering people,” said Nienaber.
“And their hygiene starts to suffer. If they forget to bathe, brush their teeth, that’s when you know that’s the start of the real decline,” said Voelker.
In order to live well with Alzheimer’s, it is important to pay attention to your health and wellness.
“The neurologist says just ‘tell yourself, is it really going to matter in the end?” said Voelker.
Even though things you once did will start to become increasingly difficult, you can still work to take care of your body, engage in mentally stimulating activities, connect with your feelings, and stay socially connected with those who care about you.
As a way to stay connected to those who are going through similar circumstances, the Alzheimer’s Association will be holding their second Walk to End Alzheimer’s this year.
“We were proud. I said ‘I am making signs and putting them on the back of our shirts so everybody knows who we are,’ and trust me, everybody knew who we were. It was fun and we did bring a lot of awareness,” said Nienaber.
Voelker and Nienaber encourage those who are caretakers to stay close to your loved ones, so you don’t miss a memory.
“I would say, just be there and provide the support and love that they’re going to need,” said Nienaber. “Just spend time with your loved ones. Especially when they have dementia, make an effort. We say, ‘I’ll go see her tomorrow,’ well tomorrow may be too late,” she added.
The Western Arizona Council of Governments (WACOG) is the local partner for resources with the Alzheimer’s Association and aging questions.
WACOG provides community presentations on various aspects of the disease for the Yuma community.
The phone number for the Western Arizona Council of Governments Area Agency on Aging is 928-782-1886.
There is also a support group that meets the first and third Friday of every month at the American Veterans Post 330 at 10:30 A.M.
As for the Imperial Valley, there is a support group at the Imperial Valley Family Care Medical Group located at 1665 S. Imperial Ave.
If you would like to volunteer your time with the Alzheimer’s Association, you can reach them at volunteer@alz.org.
